Procedures
Advanced Digestive Clinic utilise the latest technologies and techniques in medical imaging.
We offer a range of procedures including;
Gastroscopy
-
A gastroscopy (also called an upper endoscopy) is a procedure that allows your specialist to directly examine the lining of the upper part of your digestive tract, including the oesophagus (food pipe), stomach, and first part of the small intestine (duodenum). This examination uses a thin, flexible tube with a camera and light at its end called an endoscope. The endoscope is inserted through the mouth under general anaesthetic, and the upper digestive tract is inspected for inflammation (redness, irritation), bleeding, ulcers, or tumours. Certain health conditions that affect the oesophagus, stomach and small intestine can also be treated using specialised equipment.
-
Investigating symptoms such as persistent upper abdominal discomfort/pain, persistent nausea and vomiting and difficulty swallowing.
Diagnosing conditions like gastro-oesophageal reflux disease (GORD), peptic ulcers, coeliac disease, or Barrett's oesophagus
Identifying sources of gastrointestinal bleeding
Performing treatments such as stretching narrowed areas, removing polyps, or taking tissue samples for biopsy
Follow-up monitoring of previously diagnosed conditions
Evaluating abnormal medical imaging findings
-
Fast from food for 6 hours before the procedure
Clear liquids may be allowed up to 3 hours before, depending on your doctor's instructions
Inform your doctor of all medications you take, especially blood thinners, diabetes medications, or blood pressure medications
Arrange for someone to drive you home
-
The procedure typically takes 10-15 minutes
You’ll receive a light anaesthetic (sedation) through an IV line in your arm to help you relax and enter a sleep-like-state during the procedure
A mouth guard will be placed to protect your teeth
The endoscope is gently passed through your mouth, down your oesophagus, and into your stomach and duodenum
The doctor will examine the lining of these areas and may take tissue samples or perform treatments as needed
-
You'll wake up and be monitored for 30-60 minutes in a recovery area
You can typically resume eating and drinking once you are awake (within an hour)
A gastroscopy is an outpatient procedure, meaning you will be discharged home after you have completed your procedure and recovery.
You may return to normal activities the next day
-
Sore throat (Temporary)
Bleeding if biopsies were taken (Rare)
Trauma to the lining of the oesophagus, stomach, or duodenum (Extremely rare)
Reaction to sedation medication
Aspiration - inhaling stomach contents into lungs (Risk greatly reduced by carefully following fasting instructions)
Colonoscopy
-
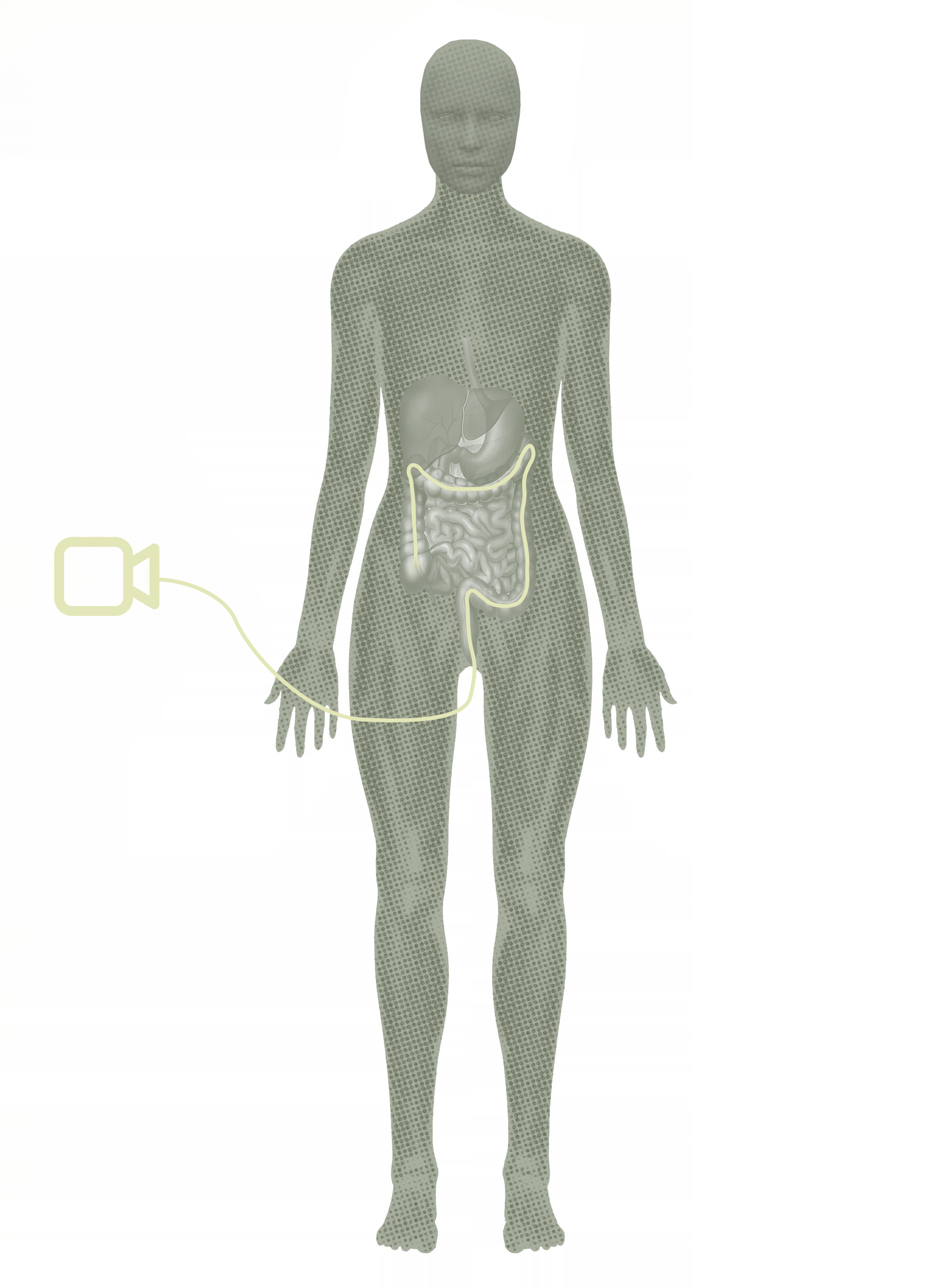
A colonoscopy is a procedure that allows your doctor to examine the entire inner lining of your large intestine (colon) and rectum using a long, flexible tube with a camera and light at its end called a colonoscope. The endoscope is inserted into the rectum under general anaesthetic, and advanced through the entire colon. During the test the colon is examined for polyps (an abnormal growth of cells in the lining of the bowel), inflammation (redness, irritation), bleeding causes, or tumours. Preparation for a colonoscopy typically involves consuming liquid bowel preparation laxatives the night before.
-
Bowel (colorectal) cancer screening
Screening for pre-cancerous polyps, including removing polyps or examining previous polyps.
Investigating symptoms such as rectal bleeding, chronic diarrhoea, changes in bowel habits, or unexplained abdominal pain
Evaluating inflammatory bowel disease (Crohn's disease or ulcerative colitis)
Follow-up assessment of previous abnormal findings
Treating certain conditions like bleeding sites or strictures
Chronic, unexplained abdominal/rectal pain
Evaluating abnormal medical imaging findings
-
Follow a special low-residue (white diet) or clear liquid diet for 2 days before the procedure
Complete a bowel preparation regimen (strong laxatives) as prescribed to clean out your colon
Stay well-hydrated with clear liquids until the cutoff time given by your specialist
Temporarily adjust certain medications as directed by your specialist
Arrange for someone to drive you home after the procedure
Wear comfortable, loose-fitting clothing to your appointment
-
The procedure typically takes 20-30 minutes
You’ll receive a light anaesthetic (sedation) through an IV line in your arm to help you relax and enter a sleep-like-state during the procedure
You'll lie on your left side with your knees drawn up toward your chest
The specialist will insert the colonoscope through the rectum and gradually advance it through the entire colon
The doctor carefully examines the lining while slowly withdrawing the colonoscope
If polyps are found, they can be removed immediately with special equipment
Tissue samples may be taken for further examination
-
You'll be monitored in a recovery area for 30-60 minutes until the initial effects of the sedation wear off
You can usually resume your normal diet after the procedure
A colonoscopy is an outpatient procedure, meaning you will be discharged home after you have completed your procedure and recovery.
You should rest for the remainder of the day
Most people can return to normal activities the following day
-
Unexpected bleeding (uncommon)
Trauma to the lining of the colon (extremely rare)
Adverse reaction to sedation
Missed lesions (small polyps or abnormalities may occasionally be missed)
Dehydration or electrolyte imbalances from bowel preparation
Flexible Sigmoidoscopy
-
A flexible sigmoidoscopy is a procedure that allows your doctor to examine the lining of the lower part of your large intestine (sigmoid colon) and rectum using a thin, flexible tube with a camera and light called a sigmoidoscope. Unlike a colonoscopy, which examines the entire colon, a sigmoidoscopy only examines the final third of the colon. The endoscope is inserted into the rectum under general anaesthetic and advanced a short distance into the colon. During the sigmoidoscopy the colon is examined for polyps (an abnormal growth of cells in the lining of the bowel), inflammation (redness, irritation), bleeding causes, or tumours. Preparation for a flexible sigmoidoscopy typically involves an enema, administered 20 minutes prior.
-
Screening for colorectal cancer or polyps in the lower colon and rectum
Investigating symptoms such as rectal bleeding, changes in bowel habits, or lower abdominal pain
Evaluating inflammatory bowel disease affecting the lower colon
Follow-up assessment of previously treated conditions
Diagnosing the cause of chronic diarrhoea
Taking tissue samples for further testing
Evaluating abnormal medical imaging findings
-
Follow a clear liquid diet from midnight the night before the procedure
Complete an enema or laxative preparation as prescribed (less extensive than for a colonoscopy)
Inform your doctor of all medications you take, especially blood thinners
You may be able to take most regular medications with a small sip of water
Arrange for someone to drive you home after the procedure
Wear loose-fitting, comfortable clothing to your appointment
-
The procedure typically takes 10-20 minutes
You’ll receive a light anaesthetic (sedation) through an IV line in your arm to help you relax and enter a sleep-like-state during the procedure
You'll lie on your left side with your knees drawn up toward your chest
The doctor will insert the sigmoidoscope through the rectum and advance it through the lower colon
The doctor examines the lining while slowly withdrawing the sigmoidoscope
Tissue samples may be taken if needed, and polyps can be removed
-
You'll be monitored in a recovery area for 30-60 minutes until the initial effects of the sedation wear off
You can usually resume your normal diet after the procedure
A colonoscopy is an outpatient procedure, meaning you will be discharged home after you have completed your procedure and recovery.
You should rest for the remainder of the day
Most people can return to normal activities the following day
-
Unexpected bleeding (uncommon)
Trauma to the lining of the colon (extremely rare)
Adverse reaction to sedation
Missed lesions (small polyps or abnormalities may occasionally be missed)
Dehydration or electrolyte imbalances from bowel preparation
Eosophageal Manometry
-
Oesophageal manometry is a diagnostic procedure that measures the strength and coordination of the muscles in your oesophagus (food pipe) that work to move food and liquids from your mouth to your stomach. The test uses a thin, pressure-sensitive tube that measures muscle contractions and relaxation of the oesophageal sphincters as you swallow.
The thin tube is inserted through the nostril under local spray anaesthetic while you are awake and swallowed down into the oesophagus.
-
Evaluating symptoms such as difficulty swallowing (dysphagia), pain when swallowing, or food getting stuck
Diagnosing motility disorders such as achalasia, diffuse oesophageal spasm, or ineffective oesophageal motility
Confirming suspected oesophageal disorders prior to surgery
Pre-surgical evaluation for anti-reflux surgery
Evaluating chest pain that may be related to oesophageal function
Assessing the function of the lower oesophageal sphincter in patients with GORD
-
Fast from food for 6-8 hours before the test
Clear liquids may be allowed until 4 hours before the procedure
Avoid smoking for at least 24 hours before the test
Certain medications that affect oesophageal motility (such as calcium channel blockers or nitrates) may need to be stopped 48-72 hours before the test
No sedation is used, so you can drive yourself to and from the appointment
-
The procedure typically takes 30-45 minutes
You'll sit upright or lie down on an examination table
Your nostril and throat will be numbed with a local anaesthetic spray or gel
A thin, flexible tube (catheter) with pressure sensors will be passed through your nostril, down the back of your throat, and into your oesophagus
You may feel some discomfort as the tube passes through your nose and throat
Once the tube is positioned correctly, you'll be asked to take small sips of water and swallow on command
The sensors measure the timing and strength of your oesophageal muscle contractions
The tube is then slowly withdrawn, completing the test
-
There is typically no recovery time needed
You can resume eating, drinking, and normal activities once the numbness in your throat wears off (usually within an hour)
You may experience a mild sore throat or nasal irritation that should resolve within 24 hours
-
Mild sore throat or nasal discomfort (temporary)
Nosebleed (uncommon)
Intolerance to the procedure (uncommon)
Trauma to the lining of the oesophagus (extremely rare)
Irregular heartbeat during tube insertion (extremely rare)
Body Surface Gastric Mapping
-
Body Surface Gastric Mapping (also known as Electrogastrography or EGG) is a non-invasive diagnostic procedure that records and analyses the electrical activity of the stomach muscles from electrodes placed on the surface of the abdomen. This test helps evaluate the stomach's electrical patterns, which control muscle contractions responsible for moving food through the digestive system.
-
Evaluating unexplained nausea, vomiting, or bloating
Investigating suspected gastroparesis (delayed gastric emptying)
Assessing chronic digestive symptoms that haven't responded to standard treatments
Diagnosing gastric dysrhythmias (abnormal stomach electrical activity)
Evaluating functional dyspepsia
Monitoring the effectiveness of medications that affect gastric motility
Researching digestive disorders
-
Fast from food for 6-8 hours before the test
Avoid alcohol, caffeine, and tobacco for 24 hours before the procedure
Certain medications that affect stomach motility may need to be temporarily discontinued (follow your doctor's instructions)
Wear comfortable, loose-fitting clothing that allows easy access to the abdominal area
No sedation is required, so you can drive yourself to and from the appointment
-
The procedure typically takes 4 hours
You'll sit comfortably on a recliner chair
The skin on your abdomen will be cleaned
A sheet containing several electrodes (small adhesive patches) will be placed on your upper and middle abdomen
The electrodes are connected to a recording device that measures electrical signals
Recordings are taken while your stomach is empty (fasting state)
You may then be given a test meal to eat
Additional recordings are taken after eating to measure your stomach's response to food
You'll need to sit still during recording periods to avoid movement artefacts
You will be able to use a handheld device, book or magazine during the test
-
There is no recovery time needed
You can immediately resume all normal activities and diet after the procedure
The electrode sites may be slightly red where adhesive was removed, but this resolves quickly
-
Mild skin irritation at electrode sites - temporary and uncommon
No serious complications are associated with this non-invasive procedure
Iron Infusion
-
An iron infusion is a procedure in which iron is delivered directly into your bloodstream through an intravenous (IV) line. This therapy bypasses the digestive system, allowing for faster and more complete absorption of iron to correct iron deficiency or iron deficiency anaemia when oral supplements are insufficient or not tolerated.
-
Severe iron deficiency anaemia
Iron deficiency that hasn't responded adequately to oral iron supplements
Inability to tolerate oral iron supplements due to side effects (constipation, nausea, abdominal pain)
Conditions that impair intestinal absorption of iron (coeliac disease, inflammatory bowel disease, after certain types of gastric surgery)
Need for rapid correction of iron deficiency (before surgery, during pregnancy, or with chronic blood loss)
Ongoing blood loss that exceeds what oral supplementation can replace
Active inflammatory bowel disease where oral iron may worsen symptoms
-
No fasting is typically required; you may eat and drink normally before the procedure
Inform your doctor of all medications and supplements you take
Your specialist will prescribe an IV iron preparation which you may be asked to pick up from your pharmacy and bring with you on the day
Report any allergies, especially to iron preparations or other medications
Wear comfortable clothing with sleeves that can be easily rolled up
Consider bringing something to read or listen to during the infusion
Arrange for transportation if you've previously had reactions to IV medications or have certain medical conditions
-
The procedure typically takes 90 minutes, depending on the type of iron preparation used
You'll be seated in a comfortable chair or reclined on an examination table
Your vital signs (blood pressure, heart rate) will be checked before starting
A nurse will insert an IV line, usually into a vein in your arm or hand
The iron solution is slowly administered through the IV line
Your vital signs will be monitored throughout the procedure to check for any adverse reactions
The rate of infusion may start slow and increase gradually if no reactions occur
Once the infusion is complete, the IV line is removed and a small bandage is applied
-
Most patients can resume normal activities immediately after the procedure
No special recovery period is needed
You may be monitored for 15-30 minutes after the infusion before leaving
-
Headache or mild fever (settles within 24 hours)
Joint or muscle pain (settles within 24 hours)
Nausea or vomiting (settles within 24 hours)
Allergic reactions (uncommon)
Anaphylaxis - severe allergic reaction (rare)
Extravasation - leakage of iron into surrounding tissue (Certain methods and extra care is used to avoid this complication as this can cause long-lasting skin discolouration)
FibroScan
-
A FibroScan is a non-invasive, painless scan that measures the stiffness of your liver to assess for fibrosis (scarring) and steatosis (fatty liver). It works using ultrasound-based technology called transient elastography, which sends a small vibration into the liver and measures how quickly it travels through the tissue. The faster the wave moves, the stiffer the liver tissue — an indicator of scarring.
This test is often used as an alternative to liver biopsy and is performed in an outpatient setting without the need for anaesthetic.
-
Evaluating for liver scarring in people with chronic liver conditions such as hepatitis B or C, alcoholic liver disease, or non-alcoholic fatty liver disease (NAFLD)
Monitoring progression of known liver disease
Screening for liver fibrosis in individuals with risk factors like diabetes, obesity, or high cholesterol
Assessing treatment response in chronic liver conditions
Helping guide decisions about further testing or treatment
-
Fast for at least 3 hours prior to your appointment (water is allowed)
Continue taking your usual medications unless otherwise advised
Let your doctor know if you are pregnant or have a pacemaker or implantable device
-
You’ll lie comfortably on your back with your right arm raised behind your head
A technician or doctor will apply a small amount of gel to the skin over your liver (right side of your upper abdomen)
A probe will be placed against your skin to send gentle vibrations through the liver
The scan typically takes about 10 minutes and is completely painless
You can resume normal activities immediately afterwards
-
No recovery time is needed
You can eat, drink, drive, and return to work or daily activities straight away
-
FibroScan is a very safe procedure with no radiation and no significant risks
It may be less accurate in people with obesity or large amounts of fluid in the abdomen (ascites)
Rarely, the scan may not produce a reliable result — in which case your doctor may recommend further testing
If you have questions before your appointment, feel free to contact your specialist’s clinic.
Have Questions About Your Procedure?
At Advanced Digestive Clinic, we're committed to ensuring you feel informed and comfortable throughout your care journey. If you have any questions or concerns about your upcoming procedure, please contact us at (02) 9426 4000.
Our experienced team is here to guide you through every step of the process, from preparation to recovery. We look forward to providing you with exceptional care.